
Dr. Milind R. Shah
Chairman, Rural Obstetrics Committee, FOGSI
E-mail: manjus@sancharnet.in, drmilindshah@gmail.com
Tutorials in Colposcopy
Contending with the Normal
Look at the picture below. A picture of a person’s lips, magnified just a little. Actually this is pretty much like doing a colposcopy. Imagine that you had to describe and certify the medical condition of this pair of lips. Unfortunately, when, as a doctor, you are asked to opine on a photograph, and issue a written report, the question of whether you will be held medicolegally responsible ‘clouds the senses’, and one has the tendency to either ask for some further investigation or give a vague answer. This happens especially with the diagnosis of dysplasia, because it is a pre-cancer.
What would you put down on paper?

Let me give you some options :
- Normal
- Some shadows around the angles of the mouth. Needs further evaluation.
- Picture is bad. No comment possible.
- Frame of a pair of lips. Base of the nose and some part of the neck included. Basic anatomy preserved. Skin over pictured area is smooth. Areas of bleached effect and corresponding shadowing probably attributable to photographic technique and limitations.
Don’t you agree that, if you had no more information about the subject in question, it would be difficult to comment on whether the lips in the picture are totally normal or not? But, if I tell you that this picture was part of a picture of a rock star, aged 26 years, who is currently one of the ‘Top of the Charts’, anyone would spontaneously say that this picture is perfectly normal. The colposcopic case shown here in this tutorial, is somewhat similar.
Look at the colpophotograph below. This lady was referred with a Pap smear saying ‘mild dysplasia’.

So, we stain the cervix with acetic acid, and later with iodine (subsequent 2 frames)

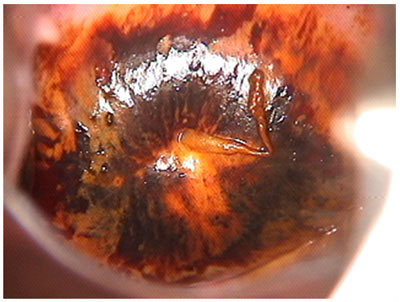
What do we see? I have had students and doctors asking if the 5 – 6 o’clock area in the upper frame is not an acetowhite area. And, some asking whether the 12 – 1 o’clock area is not iodine-negative. At this juncture, I would say, ‘step back’! Don’t get confused with micro-anatomy. Look at the case in totality. Is this woman in the high-risk category for cervical neoplasia? I should tell you here, that this colpophoto is of a 53 year old, singly married, ‘fidelous’ woman (we need adjectives in today’s day and age to indicate that the individual does not have multiple partners, besides specifying that she is married; I hope I don’t start a jihad with my infidel, unconventional vocabulary).
We decided to give her a 1 month’s course of estrogen cream vaginally, and follow-up with a repeat Pap thereafter. She did so, and the next Pap was absolutely normal. At a post-menopausal age, the number of basal cells in the Pap smear is more than in a normal smear. The nuclei are large, but regular. Still, if the age is not specified to the pathologist, it can result in the pathologist thinking in terms of ‘LSIL’ or dysplasia. Estrogen cream locally improves the maturation and restores normality to the Pap smear.
The process of neoplastic transformation begins at the squamo-columnar junction. It is therefore important to visualize the s-c junction. Well, the squamo-columnar junction is not seen in this colpophoto, so we actually would have to report that this colposcopy is inadequate. One would therefore ask : Why did we treat as we did (with estrogen cream) instead of asking for further investigation (endocervical curettage/hysteroscopy, etc) or just skirt our responsibility with a report of ‘Inadequate colposcopy-refer back to the referring gynaecologist/physician/GP’. Well, as one gets more experienced in clinical practice one comes across situations which, intuitively, one knows the answer to. In a chronically infected cervix, one which has had multiple infections (HPV and otherwise), there is bound to be some sign of an old erosion. The process of the s-c junction retreating into the endocervix would be chequered. The previous Pap smears of the patient would not have been normal. The regular look of the cervix itself is an indication that the sexual history of this patient has been simple (as opposed to ‘complex’ in a woman with many partners, or whose partner was promiscuous).
Coming back to the picture of the lips! Were we to preserve this picture (even though the picture may not be so good and even if we did not know about the person being a current rock-star!), and have a look at the face 2 years down the line, we would be able to make out if there is any change occurring. This is my contention, and I hope you agree! Similarly, I exhort all those of you, who would do colposcopy, try to produce a colpophoto of the basic unstained cervix, the aceto-stained cervix and the iodine stained cervix, in print, which the patient should keep in her medical record file. When any other gynaecologist months/years down the line examines he/she would have the benefit of comparing with the previous condition of the cervix, and this is where, I believe, half of the value of ‘Hard Copy Colposcopy’ (again, excuse the unconventional vocabulary, but I think you’ll understand) lies.
Let me touch upon the reporting of the ‘lips’. If you recognize, and are prepared to admit, most of us write our clinical findings like option a). Some of us are ‘doubting types’ and would opt for option b). If you notice, there is no way you can fault any of the options. It is obvious that option d) is the most painstaking way to report. Consider what happens as a sequel to reporting in each of the above ways.
In option a), over a long period of time, one would get ‘immune’ to the grainy quality of the print, and tend to report normality even when the print quality has precluded the diagnosis of a minor ‘dysplasia’, especially in those cases where there is a lack of correlative information.
In option b), one would be subjecting a whole lot of patients to anxiety and unnecessary further evaluation.
In option c), one would be just condemning the entire procedure, unless the reporting person took the trouble to repeat the photograph (which has cost implications).
In option d), one accepts the current photograph, and has tried to analyze it from various aspects. The first aspect, is the gross anatomy (which can be disturbed in serious disease), the second is the skin contour, which is bound to be affected, as we are concerned about epithelial changes, and lastly the quality of the photograph. This report, enthuses us to preserve this print for future reference. It also keeps us aware of the need for improvement in photographic technique. Were we to preserve this print (as I mentioned before, in spite of its faults), we might, at a later date get some more qualifying information, which would help us ‘build a case’. If a similar picture were taken after 3 years, we’d be able to compare and localize an area of change that might lead to the diagnosis of disease. It pays to be painstaking!
This would therefore essentially be a tutorial with the following intention : “Don’t imagine a tiger that isn’t there!” Remember to step back and take stock of the whole picture when faced with uncertain findings. And don’t unnerve the patient with an uncertain posture. Think of what you want to do in the circumstances and advise with aplomb. And remember, if you provide a hard copy picture to the patient, even in the event of a minor slip in diagnosis, the patient always has your hard copy downstream in time, to compare with.